For decades, the U.S. healthcare system has leaned into mass production and one-size-fits-most treatments. But for patients navigating the GLP-1 landscape—especially those without diabetes or employer-sponsored insurance—the cracks in this model have become undeniable. Amid supply shortages, surging demand, and insurance barriers, compounded medications have filled a critical gap, operating under a robust regulatory framework prioritizing safety, necessity, and individualized care.
What’s too often lost in the headlines is the why behind compounding.
Compounding Exists Because One Size Doesn’t Fit All
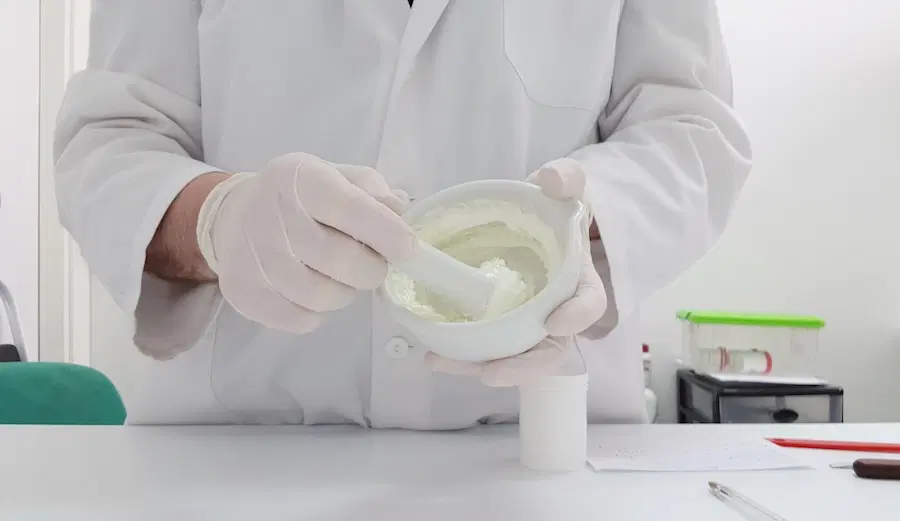
Before the pharmaceutical industrial complex took hold in the mid-20th century, most medications were compounded. Physicians and pharmacists collaborated to tailor treatments based on patients’ biology, lifestyle, and medical history. While mass-produced drugs expanded access significantly, they aren’t suitable for everyone—particularly individuals with unique physiological needs or those intolerant of commercial formulations.
Today, compounding is tightly regulated under Section 503A of the Federal Food, Drug, and Cosmetic Act, allowing state-licensed pharmacies to prepare personalized medications when commercially available alternatives are inadequate or unsuitable for individual patients. These prescriptions must be medically necessary, non-replicative, and prescribed within a valid patient-provider relationship, with additional oversight by state pharmacy boards and standards established by USP <795>, <797>, and <800>.
Compounding does occasionally face stigma due to rare cases involving noncompliant actors. However, the solution lies not in removing this vital service but in enforcing strict compliance and transparency.
The Insurance Catch-22: Why Patients Still Can’t Get Covered
Even with the rise of GLP-1 and GLP-1-GIP medications for chronic weight management, access through traditional insurance remains elusive. As of early 2025, fewer than 20% of employer-sponsored plans include coverage for GLP-1 medications intended for weight loss without diabetes, and Medicare or Medicaid coverage remains similarly limited (Healthcare Dive, 2024). Furthermore, ACA marketplace plans scarcely include GLP-1s explicitly approved for obesity treatment (KFF, 2024).
While retail prices for name brand GLP-1 medications remain high, a key issue is not cost—it’s clinical fit. Many patients are unable to tolerate or effectively respond to mass-produced formulations, underscoring the need for personalized approaches to care. Compounding plays a vital role here, enabling prescribers and pharmacists to develop customized therapies tailored to a patient’s specific biology, medical history, and health goals.
Compounded medications are not substitutes for cost-driven care—they are medically necessary alternatives for patients with unique needs who require treatment options that extend beyond what commercial products can provide.
What Personalization Really Means—And Why It’s the Next Frontier
The real promise of compounded GLP-1 therapies provides a path towards a holistic return to personalized care—not merely in chemistry, but in the entire patient experience.
Advances in health technology are fueling a renaissance in precision medicine. Wearable sensors, DNA analysis, and continuous health data monitoring are enabling healthcare providers to tailor treatment regimens based on evolving patient metrics. Physicians now have the capacity to prescribe additive formulations to preserve muscle mass, support gastrointestinal health, or enhance energy, guided by real-time physiological data rather than static dosage tiers.
This isn’t hypothetical—it’s already happening. The infrastructure supporting this evolution is rapidly expanding through specialized pharmacies, sophisticated data systems, and predictive care protocols, aligning patients with the most appropriate compounded therapies.
Compounding Isn’t a Loophole—It’s a Lifeline
Compounding might still be viewed skeptically by some. However, for countless patients, it represents the only realistic pathway to effective and tailored care. For healthcare executives and clinicians alike, compounding presents an opportunity to reimagine chronic condition treatment, shifting the focus toward prevention, personalization, and comprehensive care outcomes.
The future of medicine won’t revert to mass-market medications and fragmented care models. Instead, it will become increasingly tech-enabled, data-informed, and personalized. In such a future, compounding won’t just have a place—it will be essential to delivering treatments tailored precisely to each patient.
The critical question isn’t whether compounded therapies are here to stay. It’s whether the healthcare system is ready to fully embrace the potential of individualized care that compounding uniquely facilitates.
Chris Spears | July 9, 2025
Originally published in Healthcare Business Today
Sources:
FDA Section 503A Guidance) – U.S. Food & Drug Administration
USP Compounding Standards – USP.org
Obesity Treatment Coverage – ICER
Healthcare Dive – Coverage Gaps, 2024